
The Role of Medication in Treating Clinically Isolated Syndrome
Understanding Clinically Isolated Syndrome
Clinically Isolated Syndrome (CIS) is a term used to describe a situation where a person experiences a single, first episode of neurological symptoms indicative of multiple sclerosis (MS). These symptoms generally last for at least 24 hours and are caused by inflammation and damage to the protective covering of nerve fibers in the brain or spinal cord. Although experiencing CIS does not necessarily mean a person will develop MS, it is considered a high-risk factor for the disease.
In this article, we will explore the role of medication in treating Clinically Isolated Syndrome and discuss various options available to manage this condition. We will delve into the benefits and potential side effects of these medications, as well as the importance of early intervention for the best possible outcomes.
Early Intervention in Clinically Isolated Syndrome
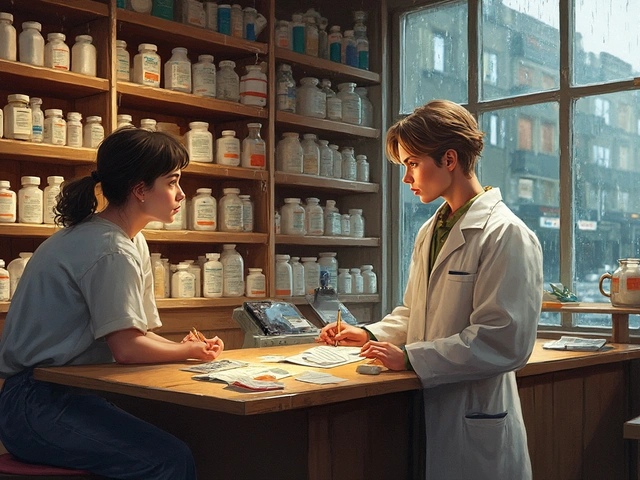
Early intervention is crucial in managing CIS, as it has been shown to significantly decrease the risk of conversion to MS. The sooner a person starts treatment, the better their chances are of preventing further neurological damage and delaying the onset of multiple sclerosis. This is why it is essential to consult with a neurologist as soon as symptoms appear, allowing for a proper diagnosis and the development of an appropriate treatment plan.
There are several medications available for treating CIS, and the choice of treatment depends on factors such as the severity of symptoms, potential side effects, and the patient's medical history. The following sections will discuss some of the most common medications prescribed for CIS.
The Efficacy of Disease-Modifying Therapies
Disease-modifying therapies (DMTs) are medications that have been proven to reduce the frequency of relapses and slow down the progression of multiple sclerosis. As a result, they are often considered as the first line of treatment for individuals diagnosed with CIS. Some of the most commonly prescribed DMTs include interferon beta-1a, interferon beta-1b, and glatiramer acetate.
These medications work by modulating the immune system, reducing inflammation, and preventing further damage to the central nervous system. They have been shown to effectively decrease the risk of developing MS in individuals with CIS, especially when started early in the course of the disease. However, it is important to note that DMTs are not a cure for MS, and their long-term effectiveness varies among individuals.
Managing Symptoms with Corticosteroids
During a CIS episode, a person may experience severe symptoms such as vision loss, muscle weakness, and coordination issues. In these cases, corticosteroids, such as methylprednisolone, may be prescribed to help alleviate these symptoms. Corticosteroids work by reducing inflammation and swelling in the affected areas of the central nervous system, providing temporary relief from the symptoms of CIS.
It is essential to note that corticosteroids are not a long-term solution, as they do not prevent the progression of the disease or the development of MS. They are primarily used to manage acute symptoms during a CIS episode and should be used under the guidance of a healthcare professional.
Considering the Side Effects of Medications
While medications can be beneficial in managing and treating CIS, it is essential to consider their potential side effects. Some common side effects of DMTs include flu-like symptoms, injection site reactions, and liver problems. Corticosteroids may cause side effects such as weight gain, mood changes, and increased blood sugar levels.
It is important to discuss these side effects with your healthcare provider, as they can help you weigh the benefits and risks of each treatment option. In some cases, it may be necessary to adjust the dosage or switch medications to minimize side effects and ensure the most effective treatment for CIS.
Monitoring and Adjusting Treatment Plans
Treatment plans for CIS should be regularly monitored and adjusted as needed to ensure the best possible outcomes. This may involve regular check-ups with your neurologist, routine blood tests, and periodic MRI scans to assess the progression of the disease and the effectiveness of the prescribed medications.
If a person's condition worsens or they experience new symptoms, it may be necessary to reevaluate the treatment plan and consider alternative medications or therapies. This emphasizes the importance of maintaining an open line of communication with your healthcare team and reporting any changes in your condition promptly.
Supporting a Healthy Lifestyle
While medication plays a crucial role in treating Clinically Isolated Syndrome, it is essential not to overlook the importance of maintaining a healthy lifestyle. Eating a balanced diet, engaging in regular physical activity, managing stress, and getting adequate sleep can all contribute to overall health and well-being.
Additionally, some individuals with CIS may benefit from complementary therapies such as occupational therapy, physical therapy, or cognitive-behavioral therapy. These therapies can help manage symptoms, improve quality of life, and support overall well-being. It is important to discuss any complementary therapies with your healthcare provider to ensure they are safe and appropriate for your specific needs.


Written by Jakob Fitzroy
My name is Jakob Fitzroy, and I am an expert in pharmaceuticals with a passion for writing. I have dedicated my life to studying medication and understanding how it affects various diseases. My goal is to educate people about the importance of proper drug therapy and prevention methods. I have authored numerous articles, providing valuable insights on medication, its development, and its impact on patients. My driving force is to contribute to the ongoing fight against diseases and improve the overall health and well-being of people around the world.
All posts: Jakob Fitzroy